查看更多
密码过期或已经不安全,请修改密码
修改密码
壹生身份认证协议书
同意
拒绝

同意
拒绝

同意
不同意并跳过






Stroke & Vascular Neurology(SVN)新近上线文章“COmbination of Targeted temperature management and Thrombectomy after acute Ischemic Stroke (COTTIS): a pilot study”,来自德国弗莱堡大学医学院、弗莱堡大学医学中心神经病学和神经生理学系Jürgen Bardutzky等。
作者团队旨在评估接受血管内血栓切除术(endovascular thrombectomy, EVT)的前循环大血管闭塞(large vessel occlusion, LVO)患者通过经鼻冷却快速降温至35℃目标温度的可行性和安全性。
LVO发病<24小时且伴有EVT指征的患者被纳入研究。患者进行EVT插管后立即开始经鼻降温(RhinoChill),并持续直至达到35℃的食道目标温度。再通后6小时内通过表面冷却维持低温,然后主动复温(+0.2℃/小时)。主要结局定义为达到35℃所需的时间,次要结局包括临床、影像学以及安全性参数。
该研究纳入了22例患者(中位年龄77岁),其中14例患者接受了额外的溶栓治疗,4例患者接受了额外的近端颈内动脉支架置入术。最后看起来正常至腹股沟穿刺的中位时间间隔为309分钟,入院至启动冷却降温的中位时间间隔为58分钟,入院至腹股沟穿刺的中位时间间隔为65分钟,入院至再通的中位时间间隔为123分钟。在30分钟(范围13~78 分钟)内达到35℃的目标温度,相当于2.6℃/小时的冷却速率。再通时,86%的患者体温≤35℃。入院时的美国国立卫生研究院卒中量表(NIHSS评分)的中位分数为15分,到第7天改善至2分,68%的患者在3个月时结局良好(改良Rankin量表mRS 0-2分)。术后并发症包括无症状性心动过缓(32%)、肺炎(18%)以及无症状性出血转化(18%)。
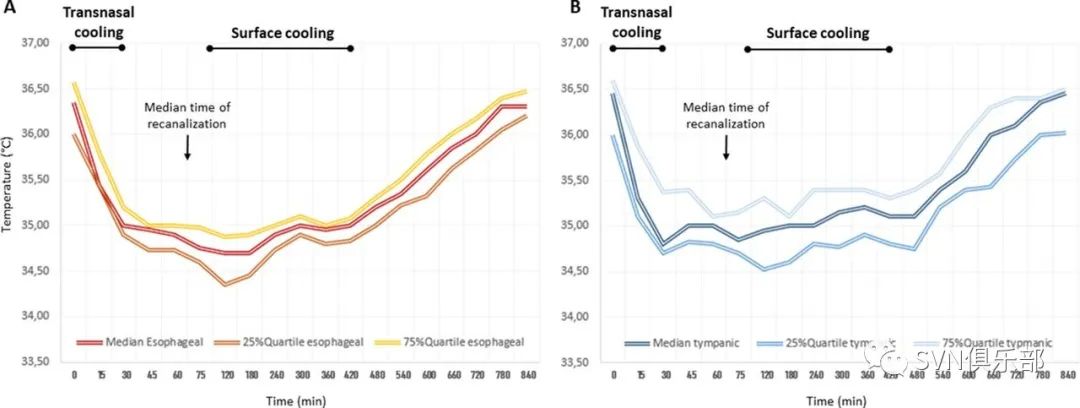
Figure 1. Oesophageal (A) and tympanic (B) temperatures in the first 14 hours of cooling induction. (A) After start of transnasal cooling (= time 0), oesophageal temperature decreased from 36.35℃ at admission to target temperature of 35℃ within 30 min. Despite halting transnasal cooling when target temperature of 35℃ was reached, temperature continued to decrease slowly (time 45–60 min). At the time of recanalisation, median oesophageal temperature was 34.9°C. Between end of thrombectomy procedure and arrival to the ICU, temperature further decreased slowly without active cooling (time 75 min). Surface cooling was started 31 min after recanalisation on ICU for 5.6 hour to reach a total duration of steady-state hypothermia of 35°C for 6 hour after recanalisation. (B) Course of tympanic temperatures did not differ significantly when compared with oesophageal temperatures, although tympanic temperatures decreased faster during transnasal cooling and were slightly above the oesophageal values during surface cooling and rewarming phase.

Figure 2. Distribution of modified Rankin Scale (mRS) score at discharge (median day 8) and after 3 months. A good neurological outcome with a mRS score of 0–2 was observed in 14 out of 22 patients (64%) at discharge, and in 15 patients (68%) after 3 months.
研究结论:低温联合血栓切除术在镇静通气患者中的联合应用是可行的。不良事件与无低温的EVT的不良事件相当。接下来将在急性缺血性卒中后靶向体温管理联合血栓切除术的试验2(COmbination of Targeted temperature management and Thrombectomy after acute Ischemic Stroke-2, COTTIS-2)中评估其疗效。

来源:SVN俱乐部
转载已获授权,其他账号转载请联系原账号
国家神经系统疾病质控中心脑血管病专业组专家撰稿,21篇脑梗死临床诊疗干货文章,精准提升脑血管临床诊疗能力!
华中科技大学同济医学院附属同济医院杨渊教授团队撰写17篇神经心理疾病临床干货文章,神经内科医生需要了解!
国家神经系统疾病质控中心帕金森病专家组倾力打造,2023年度帕金森病规范诊治能力提升培训!
脑血管病影像读图实战训练,跟随天坛医院放射科沈宓老师,练就影像读图火眼金睛!
专家共识 | 急性缺血性卒中替奈普酶静脉溶栓治疗中国专家共识
查看更多