查看更多
密码过期或已经不安全,请修改密码
修改密码
壹生身份认证协议书
同意
拒绝

同意
拒绝

同意
不同意并跳过





Stroke & Vascular Neurology(SVN)最新上线文章“Deeper cerebral hypoperfusion leads to spatial cognitive impairment in mice”,来自复旦大学附属中山医院神经内科汪昕教授、丁晶教授团队。
血管性认知障碍(Vascular cognitive impairment, VCI)是全球痴呆的第二大病因,由脑血管疾病或相关危险因素引起。然而,目前尚没有合适的动物模型可用于研究人类VCI的神经病理学变化。为了更好地了解VCI的发展,作者团队对3种慢性血管性疾病的小鼠模型进行了修饰,并进一步比较了这些模型的优缺点,有望建立一个更适合的模拟人类VCI的小鼠模型。
作者团队使用成年雄性C57/BL6小鼠(n=98),分别施以短暂性双侧颈总动脉闭塞(tBCCAO)或双侧颈总动脉狭窄(BCAS)或右侧单侧颈总动脉闭塞。在4周内检查表面脑血流(CBF)的血流动力学变化,评估空间认知障碍以明确慢性脑缺血的结果。
研究结果显示,与对照组相较,这些小鼠模型在术后1~4周显示出不同程度的CBF降低和空间参考记忆障碍(p<0.05)。作者团队发现:(1)短暂性双侧颈总动脉闭塞导致C57/BL6小鼠CBF下降90%(p<0.05),并引起急性而非长期的空间参考记忆障碍(p<0.05);(2)单侧颈总动脉闭塞引起小鼠严重的同侧缺血,产生轻微但显著的空间参考记忆障碍(p<0.05);(3)双侧颈动脉狭窄模型中,长期的CBF下降20%不会引起术后4周的空间参考记忆障碍(p>0.05),而双侧或单侧CBF下降30%可导致小鼠显著记忆障碍(p<0.05)。
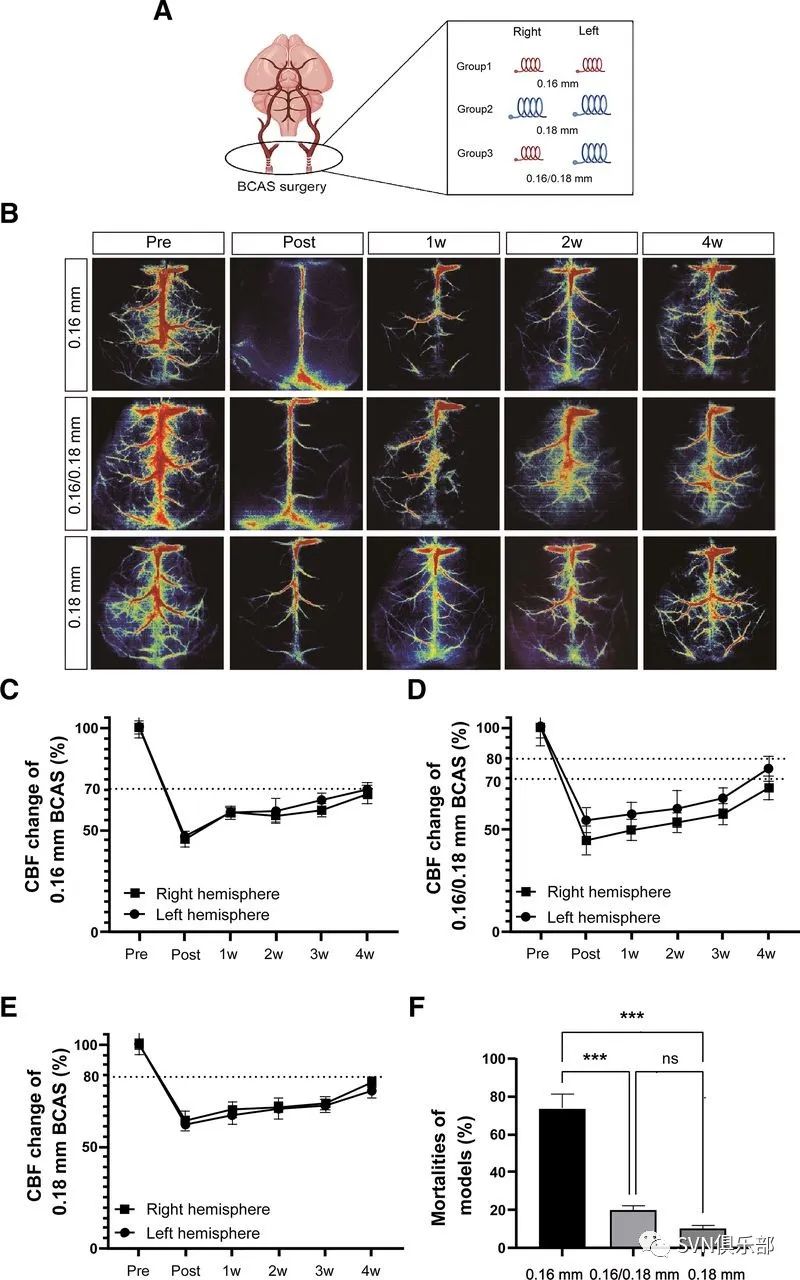
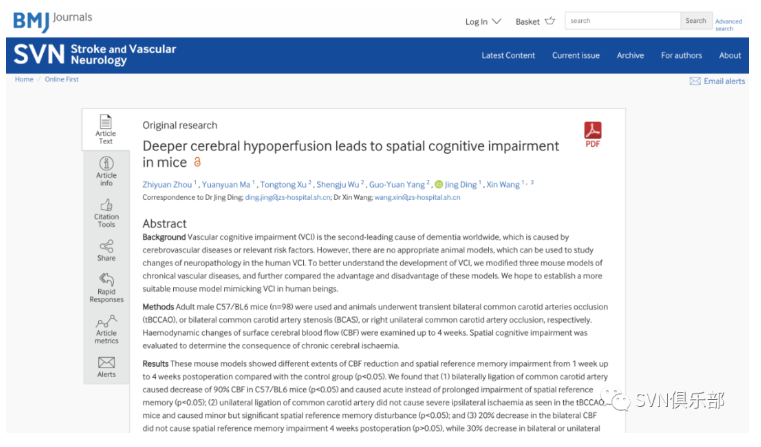
Figure 1. CBF changes and mortalities of BCAS models (A) Schematic representation of BCAS operation (grouping by different inner diameters of the microcoils). (B) Representation of laser speckle contrast image on BCAS model subgroups at preoperation, 2 hours postoperation, and 1 week, 2 weeks, 4 weeks postoperation. (C–E) Numerical representation of CBF changes measured by laser Doppler flowmetry at preoperation, 2 hours postoperation, and 1 week, 2 weeks, 3 weeks and 4 weeks postoperation. (C) The 0.16 mm subgroup of the BCAS model. (D) The 0.16/0.18 mm subgroup of the BCAS model. (E) The 0.18 mm subgroup of the BCAS model. n=5/group. (F) The mortality of different subgroups. All data were represented as mean±SEM. ***P<0.001. BCAS, bilateral common carotid artery stenosis; CBF, cerebral blood flow.
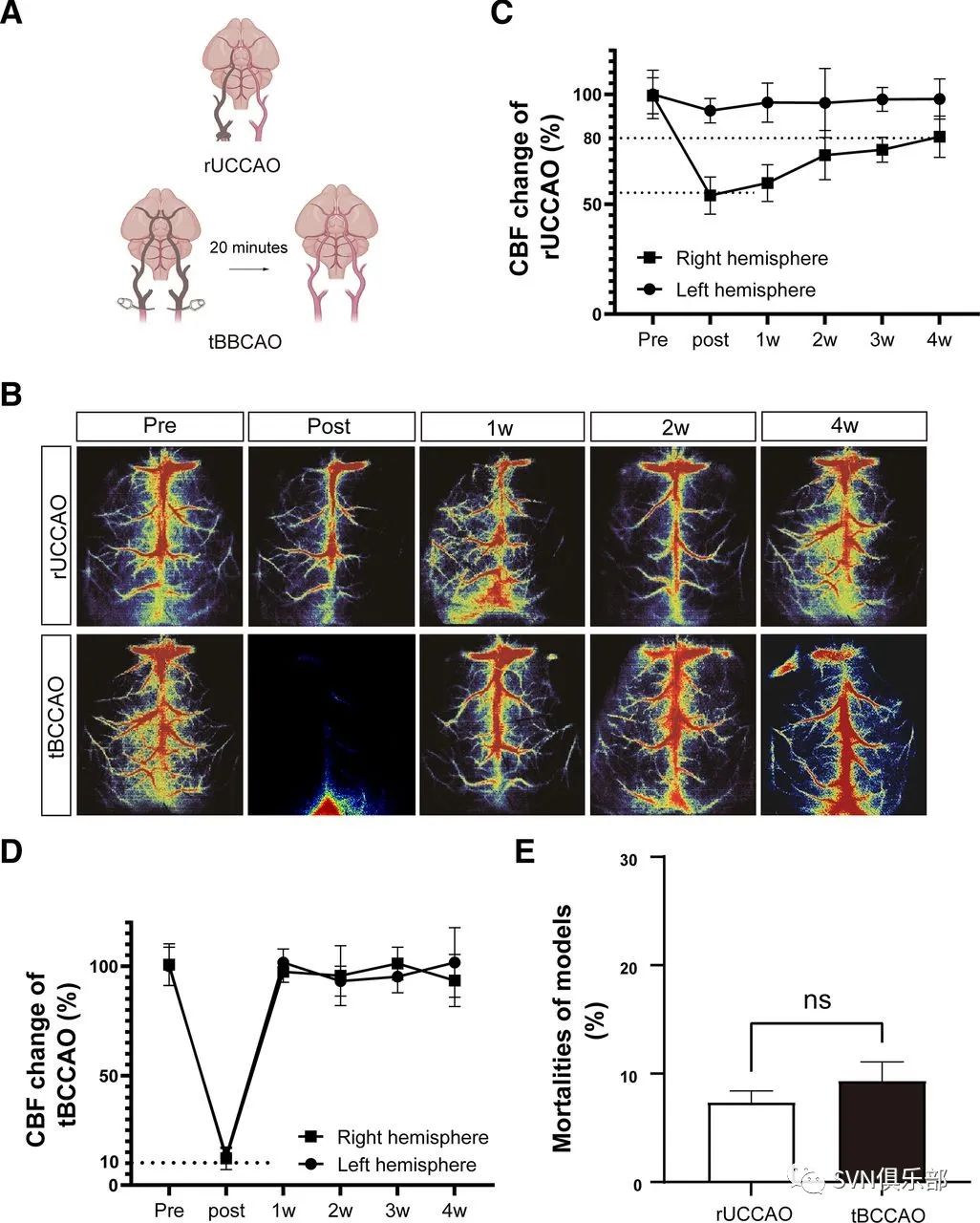
Figure 2. Cerebral blood flow (CBF) changes and mortalities of right unilateral common carotid artery occlusion (rUCCAO) and transient bilateral common carotid arteries occlusion (tBCCAO) models (A) Schematic representation of tBCCAO and rUCCAO operation. (B) Representation of laser speckle contrast image of rUCCAO and tBCCAO models at preoperation, 2 hours postoperation (rUCCAO)/immediately postoperation (tBCCAO), and 1 week, 2 weeks, 4 weeks postoperation. (C–D) Numerical representation of CBF changes measured by laser Doppler flowmetry (LDF) at preoperation, 2 hours postoperation (rUCCAO)/immediately postoperation (tBCCAO), and 1 week, 2 weeks, 3 weeks and 4 weeks postoperation. n=5/group. (C) rUCCAO. (D) tBCCAO. (E) Mortalities of tBCCAO and rUCCAO operation. All data were represented as mean±SEM. ns indicated not significant.
Figure 3. Test of spatial reference memory and motor ability deficiency of BCAS model subgroups (A) Morris water maze (MWM) acquisition period for subgroups of the BCAS model from the starting day 1 to day 5 of the test. (B) MWM probe test on day 6. (C) Times of each mouse swimming across the platform area in probe test. (D) Times of each mouse swimming across the platform area in probe test. (E) Average swimming speed of each group on day 6. All groups were compared with the control group. All data were represented as mean±SEM. ns indicated not significant; *p<0.05; **p<0.01; **p<0.001. 0.16 mm subgroup (n=7); 0.16/0.18 mm subgroup (n=10); 0.18 mm subgroup (n=11); control group (n=12). BCAS, bilateral common carotid artery stenosis.
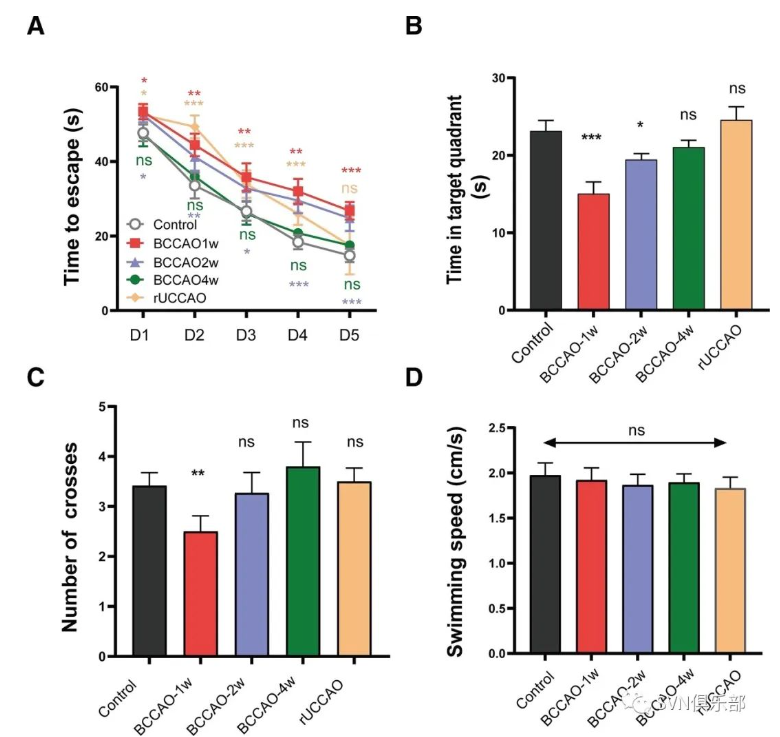
Figure 4. Test of spatial reference memory and motor ability deficiency of right unilateral common carotid artery occlusion (rUCCAO) and transient bilateral common carotid arteries occlusion (tBCCAO) models. (A) Morris water maze (MWM) acquisition period for tBCCAO at 1 week, 2 weeks and 4 weeks after operation from day 1 to day 5. (B) MWM probe test on day 6. The time each mouse swimming in the quadrant including the platform area. (C) The time each mouse swimming across the platform area in probe test. (D) Average swimming speed of each group on day 6. All data were represented as mean±SEM. All groups were compared with the control group. NS indicated not significant; *p<0.05; **p<0.01; ***p<0.001. tBCCAO 1 week, 2 weeks, 4 weeks group (n=11/group); rUCCAO group (n=12); control group (n=13).
研究结论:在研究VCI的机制和发展治疗方法时,作者团队证明了使用0.16/0.18 mm微线圈的BCAS可作为一种替代的VCI小鼠模型。

来源:SVN俱乐部
转载已获授权,其他账号转载请联系原账号



血栓预防及血栓形成的治疗推荐丨2022 AHA/ASA自发性脑出血患者管理指南
指南共识 | 特发性正常压力脑积水临床管理中国指南(2022)
脑出血发病机制的诊断评估丨2022 AHA/ASA自发性脑出血患者管理指南
查看更多